|
|
|||
|
The
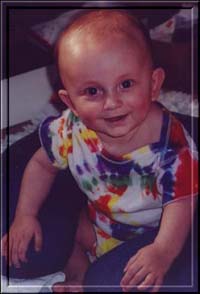
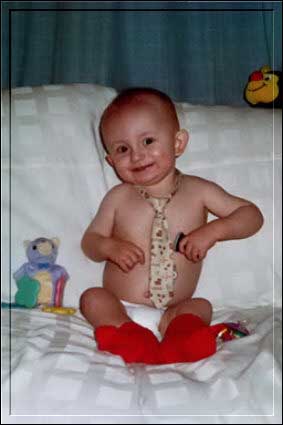
Story of The Mighty Quinn
Written
in early 2002
Only one thing stood out as being even slightly out of the
ordinary: every time I tried to feed him, he would only latch on for a
second, then stop and cry. I called the nurse who had assisted in the
birth, Judy Breitenfeld, toward the afternoon of the first day of
Quinn’s life. I told her he wasn’t eating. She said not to worry,
this is common for babies - they don’t always eat at first. She’d
be over day after tomorrow to check on him, she was sure all would be
well by then.
The second day he didn’t eat, either, though, and by the
second night I had begun to have the overwhelming feeling something
was very wrong. I attributed it to myself - my own feelings of
inadequacy as a new mother. I
must have been doing something wrong in my efforts to get him to feed
– maybe my breasts were too big or I was holding him wrong. He cried
hard that night, looking me straight in the eye as he did – as if he
were trying to tell me something, it seemed.
I felt that, but I didn’t know what it was he was trying to
say to me. His breathing seemed really fast somehow – was this
normal? Maybe he was dehydrating.
Judy was due to come at 9 o’clock the next morning, but was
delayed until 11. By then, Quinn was looking a dusky gray. He was
having trouble breathing and STILL hadn’t eaten anything, and was
continually crying. Judy walked in, took one look at him and suggested
we go to Cardinal Glennon Children’s Hospital. She knew the
lactation consultant there, and she called ahead to let her know we
were coming and to have someone ready. In my mind Quinn was
dehydrated, we would get him to the hospital, they’d get an IV in
him and get him hydrated, then I could speak with the lactation
consultant about what I was doing wrong and remedy the situation.
Everything would be fine.
On the way to the hospital, Quinn had even more difficulty
breathing, and by the time we took him out of the car, his eyes had
begun to roll up into his head – he was going into shock. We
didn’t know that at the time, however, just…things seemed very
wrong, and we were glad to have brought him there. We went in to the
hospital and as planned, there were two nurses there waiting for us
with Denise, the lactation consultant. We went right up to them and
showed Quinn to them. Patty, the supervising nurse, took one look at
him, swooped him into her arms calmly, and took him upstairs to the
NICU. The other nurse, Michelle, stayed with us and took us to the
NICU waiting room to wait for him.
Patty was so calm I didn’t really suspect she was worried,
just that she wanted to get him taken care of, but nonetheless, as
soon as she took him, I broke down and cried. Josh had been parking
the car and he came upstairs with us when we went. In some ways things
became a blur after this, and in others they are emblazoned clearly in
my mind.
Judy
sat in the waiting room with us to keep us company and to make sure
both Quinn and we would be okay. When Michelle DID bring us into the
NICU she took us into a room with Patty and several other people I
assume were maybe students or something – Glennon is a teaching
hospital. At the time I hardly even noticed them, but looking back I
seem to remember this room being quite crowded. I think Denise and
Judy may have been in there with us – I cannot be sure.
I
know Patty had said something about Quinn’s heart prior to this,
something about the cardiologist wanting to talk with us. It didn’t
really register with me, although Josh was beginning to worry. Dr.
Balfour came in them and spoke very seriously and clearly to us,
although he could have been singing the ABC’s for all I registered
– somewhere in my mind I had shut down and was looking at everything
as if from the outside – I was convinced I was dreaming. He was
saying something about a heart defect, and I looked over at my husband
who was weeping openly. Some part of me wondered why he was crying.
This is an odd dream, I thought.
Dr. Balfour began to draw a diagram of Quinn’s heart and
explain what the problem was – Hypoplastic Left Heart Syndrome. A
leaky tricuspid valve. He explained very clearly, I remember, though
to me he may have very well spoken Greek for all the good it did me. I
was just convinced they were lying – they had the wrong family, they
had us confused with someone else, this was a dream. I tried very hard
to listen to what they were saying to us, but I kept looking at the
bordered design of the wallpaper at the top of the wall – the little
children standing together pointing at the Cardinal Glennon logo,
repeated over and over all along the top of the wall.
Josh
seemed so upset – I watched their faces as they spoke to us, telling
us why Quinn’s heart was overdeveloped on one side and
underdeveloped to the point of uselessness on the other. They were
explaining our options. Transplant, a 3-staged surgery, or
“compassionate care” (i.e. – take him home and let him die). At
some point I did manage to digest “most serious heart defect” and
that my son’s life was at stake. I was in shock, denial, all of it.
He was just dehydrated, I thought, how did this happen?
We’d
get to the hospital around 7 am and leave around 9 or 10 pm,
emotionally and physically exhausted, not knowing how much time we may
even have with our son, would he even qualify to have these surgeries
we were so counting on. We spent our days with him being as positive
as we could for him – we spoke to him to let him know we were there,
we read him Harry Potter books, we touched him and gently stroked him.
We
constantly questioned the doctors and nurses in charge of his care.
Was this somehow our fault? No, this is a very random heart defect as
far as anyone knows. There is no way to either predict or prevent it.
It is only usually detectable by a Level 2 ultrasound, which is only
done if there is some complication during pregnancy, some cause to
look at the heart. As my pregnancy was perfect, there was no reason to
question it.
We
had questions every day for them, and they patiently answered every
one of them, all the while taking the most gentle and brilliant care
of our son, and for that matter, of us. They were never bothered by
our constant vigil at his bedside, or the reading of the Harry Potter
books, or the barrage of questions, or the steady flow of people who
came to visit and support us.
Each
day we waited. We waited for Quinn to slowly fight off the infections,
we waited for him to get stronger, to be healthy enough to qualify for
the surgeries. Our lives were lived in the hospital at his bedside –
we scarcely left to eat or use the bathroom. We had no idea if he
would live or die, and we didn’t want to chance missing any time
away from him. We wanted to be with him always.
The
following day the neurologist visited with a surprised expression on
his face. Quinn had small pitikia in his brain, but they were minimal,
and he may grow out of any damage he suffered. He would be able to be
independent and his cognitive abilities had not suffered as far as he
could tell. He was okay, and furthermore, the incident had NOT
affected his candidacy for the Norwood. Onward, ho.
The
surgery was scheduled for November 2nd, when Quinn was 12
days old. IT is usually done at about 5 days old, but in light of
Quinn’s circumstances they had to wait for him to be healthy enough
to undergo such a procedure. We arrived at 7am that day in order to
kiss and hug our little man before he went off to the table. Tense
does not begin to describe the atmosphere. We parked ourselves in the
OR waiting room in readiness to wait.
The
surgery was described to us by Dr. Fiore, the cardio thoracic surgeon:
they would slow all of Quinn’s vital functions and put him on the
heart/lung machine, which would keep his body alive while they
performed the surgery. His head would be packed in ice; the ventilator
would do his breathing. They would stop his heart in order to clear it
of blood while they worked. The surgery itself would take about 15
minutes – all they had to do was place a shunt into his heart to
keep it working until the next surgery. The surgical nurse, Barb,
would keep us updated during surgery as to where they were in the
process.
The
surgery went smoothly, and all day Barb kept us updated with,
“nothing is really happening, things are going smoothly,” which
kept us happy, because in this case, no news really was good news. It
was an uneventful, and therefore a good day of waiting for us. Quinn
did splendidly.
At
the end of the long long day Dr. Fiore came out and let us know how
things went. He told us he had been unable to fix Quinn’s leaky
tricuspid valve as he had intended. The reason for this is that when
he got in there to fix it, he saw that the valve was an A/V canal
valve, which meant that instead of the standard 3 leaflets, there were
about 13…or some number like that. It would be like trying to sew
wet tissue paper and he would do more harm than good to try to fix
them, so he went ahead and left the valve alone, saying he would fix
it at the next surgery when Quinn, and his valve, were bigger. Other
than that everything was smooth. It was finally time for us to see
him.
Quinn
was on a ventilator that was essentially breathing for him, also due
to the paralyzing medication and the sedative. He was on much fentanyl
for pain, with a sedative and maybe another pain medication as well.
He was also on several heart medications to help his heart function.
In other words, there were a great many pumps and machines hooked up
to him. He had two pacer wires coming out of his chest that could be
used in an emergency to start his heart if necessary.
He had drainage tubes as well to drain the excess blood off of
his heart, and a Foley catheter for urine output. Then of course the
standard leads to keep track of his heartbeat, his oxygenation level,
and his blood pressure, all of which showed up on a big monitor
overhead so we could watch it and have our blood pressures rise and
fall with Quinn’s.
The
next day he was doing better, and he improved steadily after that,
coming off of the vent within about 5 days. It was a little longer
than the doctors would have liked, but better safe than sorry, and he
needed the extra help for a while. Once he did come off the vent,
though, there were no problems. His recovery went fairly smoothly.
We
were in the hospital for almost another three weeks after that. His
chest was closed, but got an infection in the wound, so they re-opened
the wound and left it open to heal, changing the dressings three times
a day and irrigating it with saline. He also had a NG tube through
which he was mainly fed, still not having gained enough strength to
eat on his own – at least, not enough to sustain himself.
We
took Quinn home on Captopril, Lasix, baby aspirin, Digoxin, and NG
tube, and dressing changes three times a day. It had been a month
since he had been here, born here, and we were elated to have him back
home where he belonged. We didn’t even mind the schedule changes of
around the clock feedings and meds. He took really well to sleeping at
home with us, in our bed – he slept more peacefully than I’d ever
seen him sleep, as did we. And amazingly, he slept through the night.
Quinn’s
second surgery, the Bi-Directional Glenn, was scheduled for February
19th. He was 4 months old. Normally the surgeons like to
wait until a baby is about 6 months old before doing this surgery, but
because of Quinn’s leaky tricuspid valve and all the work his heart
had to do to compensate, Dr. Fiore opted to do it then. Quinn was
gaining weight well and was prime and ready for surgery. And for us,
the sooner the better, we wanted to get it all over with so we could
go home and live a “normal” life for awhile.
So
the G-tube surgery was a breeze compared to the other two – we were
only in a week that time if even a week. His little stomach just had
to heal and he had to get used to the food going straight through to
his stomach and they needed to make sure he could tolerate feedings
okay. He did – our little Mighty Quinn, he was so used to this
healing process he gave no problems and again we went home.
This
year I think we will have no surgeries – the first year ever of no
surgeries – and probably early next year he will be having his
Fontan, the completion of the 3-stage procedure to re-route his
circulation. For now, we just enjoy every second of our “normal”
life together.
Namaste’
Echota ***UPDATE***
We DID have a "normal" life together there for a long while, and one whole year of no surgeries. That was 2002. Then in 2003 we knew the cath was coming to look for what would need to be done with the Fontan. But we also knew that his tricuspid valve regurgitation was getting worse, and eventually after the cath, we found out that we would not only need to try and repair or replace it, but do it then, ASAP. My heart sank. My inner me knew that that was it - my first thought was that I wasn't ready to give him up so soon, I wanted more time. I didn't say it aloud, though. because the practical me also knew that I had to do this, because if I didn't give Quinn every chance I knew I could, I would never forgive myself and would always question my actions. So I knew I had to release him into the care of the doctors and into the hospital. So June 3rd, 2003, we went in for Quinn's surgery. One the weigh-in and vitals and shower were done, I got to hold him in my arms for an hour before he had to go in for surgery. That was the last day we saw him smile.
He didn't die in my arms, but he died holding my hair (his source of comfort) and with me stroking his head and whispering in his ear that I loved him and that I was there. I watched him take his last breath and I knew he was gone, just as I knew the doctors and nurses had to do all they could to try and revive him. June 9th, 2003, Quinn gave up his fight and let go. Half a heart is one thing, but half a heart without a valve is another entirely. He just couldn't do it.
Quinn was
our greatest joy and our greatest inspiration. I will always cherish
every second I had with him, and will always be grateful for the time
I got to share with him. He was my true Hero, my Mighty Quinn.
|
|||
|